How would you feel, when you're told, you won't be able to give birth because your ovaries have run out of eggs, especially when you're in your twenties?
Joy News Medical Correspondent, Neta Kris Abiana Parsram navigates the story of a victim, exploring her fears, frustrations and interventions available.
Ewuresi Nkrumah, 27, a sales attendant has been experiencing irregular periods for years but in August 2021, her body had turned off the taps.
As if that was not enough, hot flashes will not let go of her.
After visits to several health facilities, in December 2021, Ewuresi was finally diagnosed with early menopause.
“They told me, my 27-year-old ovaries were acting like that of a 50-year-old. They said it was shutting down.
“All I've known is that women who are older and have finished their families are the ones who experience menopause. Me? How did this evil find me?
"I'm only 27 years old. I'm not even married. Honestly, my mind is muddled. I’m trying so hard not to think about it,” Ewuresi couldn't hide her frustration.
The fertility clock
Menopause is a natural transitional process in women’s lives where they experience a decline in reproductive hormones and eventually fertility.
It usually occurs between the ages of 49 and 52 years.
BMC Women's Health states that, approximately 4.2–7.6% of women worldwide experience menopause at ages before age 45.
Early Menopause usually occurs between 40–45 and Late Menopause beyond 55 years.
It has been found that early or late menopause may be associated with higher risk of heart disease, bone weakness, and breast and uterine cancers.
Premature ovarian insufficiency (POI) on the other hand is the loss of normal ovarian function before age 40.
This condition affects approximately 1% of women under 40 years old and 0.1% of women under 30 years old.
A small percentage, nonetheless, the individuals who fit in this category are isolated and anxious for fear of stigmatisation.
Premature Ovarian Insufficiency is marked by the cessation of menstruation, as well as changes in the hormones that regulate the menstrual cycle. These changes usually result in loss of fertility.
According to an article published in F1000 Research in 2020, the condition is characterized by deficient ovarian sex hormones and decreased ovarian reserve, which together lead to an accelerated reduction in ovarian function and an early onset of menopause.
Dr. Edem Hiadzi, a consultant obstetrician and gynaecologist and founder of Lister Hospital in Accra noted that a woman's biological clock is independent of age.
“Most people assume your biological clock goes with your age. It is not necessarily so, it goes with your ovarian reserve. The ovarian reserve varies from woman to woman. It is the reserve which then declines with age,” he explained.
A 2021 article in the Journal of Ovarian research says “Ovarian reserve” is a term that is used to describe the remaining capacity of egg cells in the ovary. With age, the ovarian reserve tends to naturally diminish.
Dr. Hiadzi expanded on the variability of the ovarian reserve with some statistics.
“80% of women will come with an average ovarian reserve. 10-15% may have too many eggs; these are more prone to a condition known as Polycystic Ovary Syndrome (PCOS). 5% fall in the premature ovarian failure category.
“Depending on the group you belong to, you may be looking at your colleague who is having a child at 39 years and think, ‘I'm only 34 and I have more time.’ It might not be so for you,” he emphasized.
What to look out for
Symptoms of ovarian insufficiency are highly variable and often indistinguishable from those seen in menopause or other low estrogen states.
Ewuresi explains that some symptoms could have driven her to the hospital earlier, however since she had little knowledge, she did nothing.
“Even if I missed my period for 3 months it would eventually come so I didn't think much of it.
“I went to see the doctor because of the sudden feeling of feverish heat I keep having. It is becoming unbearable and often makes me anxious and uncomfortable in my surroundings.
“The doctor asked so many questions and requested several blood tests. Initially they thought it was a thyroid issue. I never imagined it had anything to do with my ovaries,” she recalled.
On the word of a paper published in the frontiers in Cell and Developmental Biology, some symptoms experienced by women with POI include hot flashes, painful sexual intercourse, night sweats, dry eyes, decreased sexual desire, having difficulty conceiving, and experiencing new-onset menstrual irregularity,
Elucidating the cause of POI is most relevant in diagnosing and treating affected women.
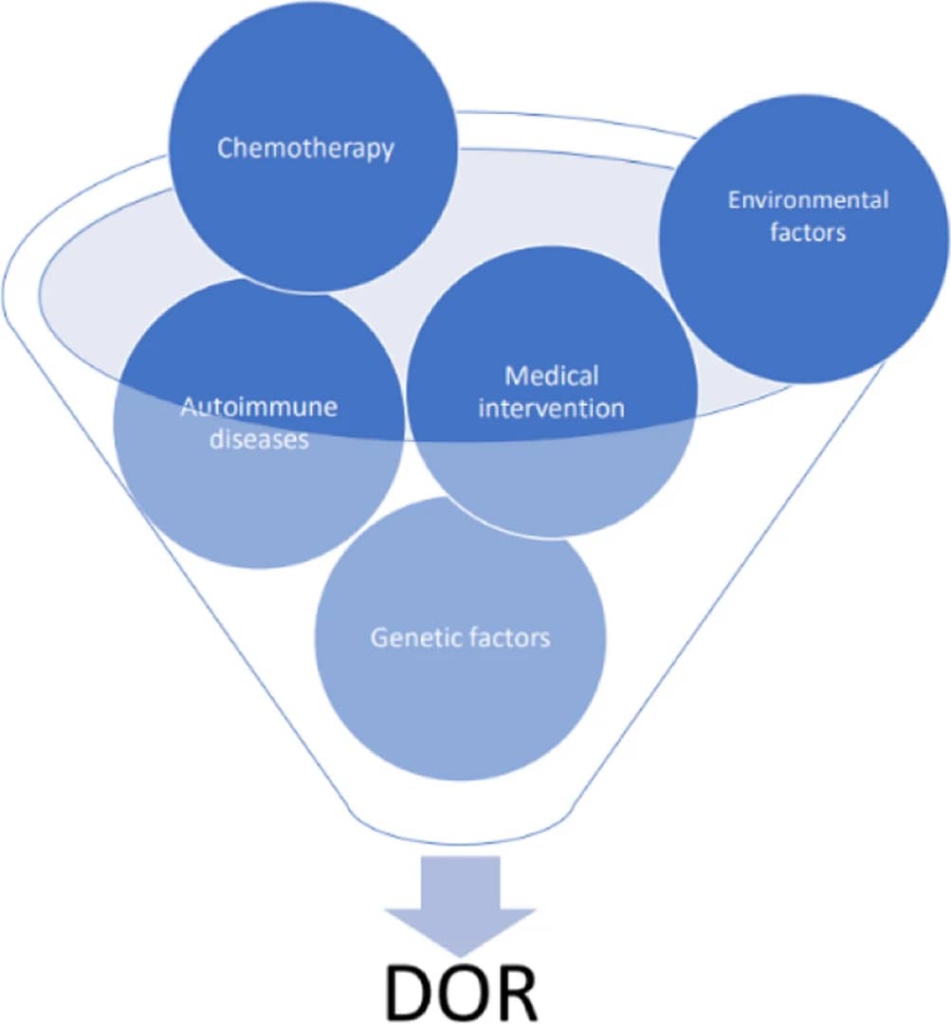
Research overtime has revealed that aside from the unexplained proportion of small ovarian reserve, generic factors, autoimmune diseases, environmental factors, social choices, and more can influence the state of the ovarian reserve.
“Several specific genetic markers have been identified to be associated with ovarian reserve depletion through numerous important pathological pathways.
Some of these manifest as syndromes, like those seen in Turner's syndrome and Fragile-X syndrome,” Dr. Hiadzi said.
It has been noted in some research works that a history of ovarian surgery can reduce ovarian reserve due to injury to blood vessels supplying the ovaries, infection after surgery, and blockage of small blood vessels by clots.
Specialist Obstetrician Gynaecologist, Dr. Yaw Owusu Gyanteh has this to say on the matter.
“Ovarian surgeries are usually done for removal of uterine tissues planted in and around the ovary or other fluid-filled masses called cysts.
“Whether the surgery is done under camera guidance through a small cut or by open surgery, normal ovarian tissue containing functional follicles can be inadvertently removed irrespective of the skill of the surgeon.
He added certain surgical instruments can lead to death of the ovary.
“The use of an electrosurgical coagulation instrument known as a diathermy during the procedure may also cause damage to the ovarian tissue and blood vessels which may lead to reduced blood supply (ischemia) to some parts of the ovary eventually leading to loss of ovarian tissue.
“This loss of healthy ovarian tissue from inadvertent removal, destruction by coagulation and the damage to vessels reduces the healthy follicular pool, therefore, reducing ovarian reserve,” he explained.

Endometriosis is a condition in which tissue resembling that which grows in the uterus develops in other areas of the body. It is one of the factors affecting ovarian reserves particularly in young females.
The Journal of Reproductive Biomed links a decreased ovarian reserve to endometriosis.
Body Mass Index (BMI), a marker for obesity also affects ovarian reserves by changing the hormone levels of women.
Many studies have shown negative effects of obesity on ovarian reserves.
In a recent report, underweight prevalence amongst women of childbearing age was seen to decrease by about 45% from 1993 to 2014 and projected further decline to reach 2.2% by 2030.
Obesity conversely has significantly increased by over 400% from within the same number of years. By 2030, nearly 23% of Ghanaian women are estimated to be obese.
These figures are not encouraging especially when looked at in the light of fertility.
The International Journal of Gynaecology and Obstetrics and the International Journal of Reproductive Biomedicine both impressed that ovarian reserve is affected by various non-genetic factors as well.
These include poor sleep quality, alcohol drinking, cancer drug use, exposure to radiation, and most commonly age.
Dealing with the condition
Ewuresi voices out her struggles with the diagnosis and finding support.
“The doctors say it is not a curse, but my aunties look at me with strange glances. Already, I feel less like a woman knowing I can never have children of my own.
“My parents have been really supportive. Sometimes my heart breaks for them. I'm an only child. This means they will never be grandparents.
“The initial weeks after the diagnosis were very difficult. I felt worthless. Why would any man consider a woman who can't make him a father? I felt less attractive.
“Thoughts of taking my life sparingly occupied my mind. I tried not to entertain them because my parents tried so hard to cheer me up,” she lamented.
Social and cultural expectations often cause us to be harder on ourselves than is necessary.
Concerns about the perceptions others have and how they are likely to treat us once they have knowledge about who we truly are makes us walk on eggshells as shadows of ourselves.
Dr. Caleb Ansah, explains how such diagnoses are received.
“The most common words women use to describe how they feel in the hours after getting the diagnosis of POI are “devastated,” “shocked,” and “confused”.
“Clearly, the news propels some patients onto a difficult journey.
“POI is a serious and incurable chronic disease. The diagnosis affects a woman’s physical and emotional well-being hence, management of the condition must address both.
“Patients face the shock of the diagnosis, associated stigma of infertility, grief from the death of dreams, anxiety from the disruption of life plans, confusion around the cause, discomfort from symptoms of estrogen deficiency, worry over the associated potential medical complications to follow, and the uncertain future that all of these factors create,” he said.
Dr. Ansah went on to point out ways to better manage individuals in such predicaments.
“There is a need for an evidenced-based integrated program to assist women with POI in navigating the transition to acceptance of the diagnosis, ongoing management of the condition, and ongoing maintenance of wellness in the presence of the disorder.”
He added: “A health-centred approach can gradually replace the disease-centred approach and put patients in partnerships with professional healthcare providers.”
“Ideally, the journey transitions each patient from seeing herself as a victim, to a survivor, to a woman who is thriving.”
Ice on the eggs: the fertility insurance
Mavis, 45, has been married for almost 20 years without a child.
Her numerous attempts at IVF proved futile.
“I have been trying for more than 15 years to have a child. I have taken too many tests. I tried IVF three times, all failed. At one point I got so discouraged. I would wet my pillow in tears.
“Recently, I heard from a friend, I could freeze my eggs. I wasn't sure it was possible in Ghana. Hmmm, I hope it’s not too late for me," she exhaled.
Criticized as exploitation yet extolled as empowerment of women, egg freezing is a contested reproductive technology that has brought the human egg into the limelight.
Egg freezing, more technically referred to as oocyte cryopreservation, and involves the use of hormones to stimulate the ovaries in order to mature the eggs for retrieval and subsequent freezing and storage.
It is an option which is gaining popularity in recent times especially for women who know they want to have children but are not currently ready.
The Society of Assisted Reproductive Technology (SART) estimates that the survival rate of human eggs after freezing and thawing is 90%–97%, the fertilization rate is 71%–79% and the implantation rate is 17%–41%. These statistics, however, are for women younger than 30 years.
The Canadian association Journal also states that “Pregnancy rates decline with advanced maternal age at the time of freezing.” In other words the earlier you have your eggs frozen the better.
Not many studies have been done in Africa on the topic as it is a fresh technology still gaining ground.
Dr. Edem Hiadzi has been working with countless individuals on their journeys with assisted reproductive technology for several years.
He advises, “The biological clock is there; you need to know which group you belong to. Knowing your ovarian reserve can help you decide.

If you know the reserve, you can then know when to store it.
If you're not ready to have children yet, then the earlier you get your eggs stored, the better,” he said.
He continued, “Now there are very good storage techniques available right here in Ghana that can keep eggs for a very long time. We are able to store for about 10 years. We may go beyond that in the future. You can always store while searching for Mr. Right.”
“If you find Mr. Right and your reserve is preserved then you can either donate your egg to somebody or request for it to be destroyed for you. It's just like insurance,” he said.
Dr. Hiadzi also addressed the concern of egg depletion from the procedure.
“You cannot store the eggs of next year today. Storing your eggs does not mean they will run out.
“Only what is available for that month can be stimulated to maturity and harvested,” he said.
“For women who are advanced in age and are unable to carry their own pregnancy, surrogacy is another option. This is more like renting a younger person's womb to carry the pregnancy. That also comes with its costs,” he concluded.
The cost of insurance
The process of cryopreservation of human eggs involves taking into consideration the cost of ovary stimulation, egg harvesting and the yearly cost of freezing.
Specialists in the field explain that Stimulation cost depends on the ovarian reserve, which in turn determines the number and strength of medications required for the cycle.
As a result, the cost for stimulation is individual-dependent.
Sometime last year, a single cycle was estimated to cost $10,000 which today averages about GH₵ 80,000.
The cost of freezing per year is about GH₵ 3,500. This means if you choose to store your eggs for 5 years, you will be required to pay the amount yearly to extend the storage time.
Though it is available it's expensive and hence not readily available.

Dr. Hiadzi says “a lot of things can be postponed but not pregnancies at the right time.”
There have been numerous debates on whether to start recommending ovarian reserve checks for women generally.
The concern, however, has been that it may put too much pressure and stress on women.
Is there really any point in determining your reserve, if the options available, should you have a small reserve, are inaccessible?
Will knowing your ovarian reserve bring peace or unrest?
A stronger effort from government, health care professionals and stakeholders to establish suitable policies as well as recognize new and creative interventions that are cost-effective, culturally acceptable, and sustainable and can easily be integrated into the Ghanaian health system to curtail the phenomenon of failing eggs.
Latest Stories
-
Kwesi Yankah: Escape from Ghana
3 mins -
Musician DeThompson DDT drops new single Happiness
9 mins -
Ukraine’s Grain Initiative raises over $200m, provides lifeline amid global food crisis
1 hour -
Dancehall queen Spice donates to students of 3 basic schools in Accra through MYO Global Foundation
1 hour -
Kamal-Deen Abdulai urges Nanton to help NPP break the 8
2 hours -
TVET is not a dumping ground for underperforming students – C/R Minister
2 hours -
BoG Governor calls for increased preparedness to respond to emerging financial sector challenges
2 hours -
IGP calls on public to aid Police in ensuring peace during 2024 election
2 hours -
Miner jailed, fined for stealing motorbike worth GH¢13,500
3 hours -
Dozens killed in Pakistan sectarian violence
3 hours -
Police place GH₵20K bounty on group over election violence threats
3 hours -
From classrooms to conservation: 280 students embrace sustainability at Joy FM/Safari Valley’s Second Eco Tour
4 hours -
Jordan Ayew’s late goal not enough as Leicester lose at home to Chelsea
4 hours -
Global Crimea Conference 2024: Participants reject Russian claims to Soviet legacy
4 hours -
Jospong Group, Uasin Gishu County sign MoU to boost sanitation services in Kenya
5 hours

